Introduction: Herd Immunity and Vaccination
The concept of herd immunity has been a focal point in global health discussions, especially in light of the COVID-19 pandemic. But what does herd immunity truly mean, and why is it so closely linked to vaccination? Understanding this relationship is vital to public health strategies and efforts to control the spread of infectious diseases. In the United States, achieving herd immunity is key not only to defeating COVID-19 but also to addressing various preventable diseases that can overwhelm healthcare systems. This article delves into what herd immunity is, how vaccination helps achieve it, and the current state of vaccination efforts in the US.
What is Herd Immunity?
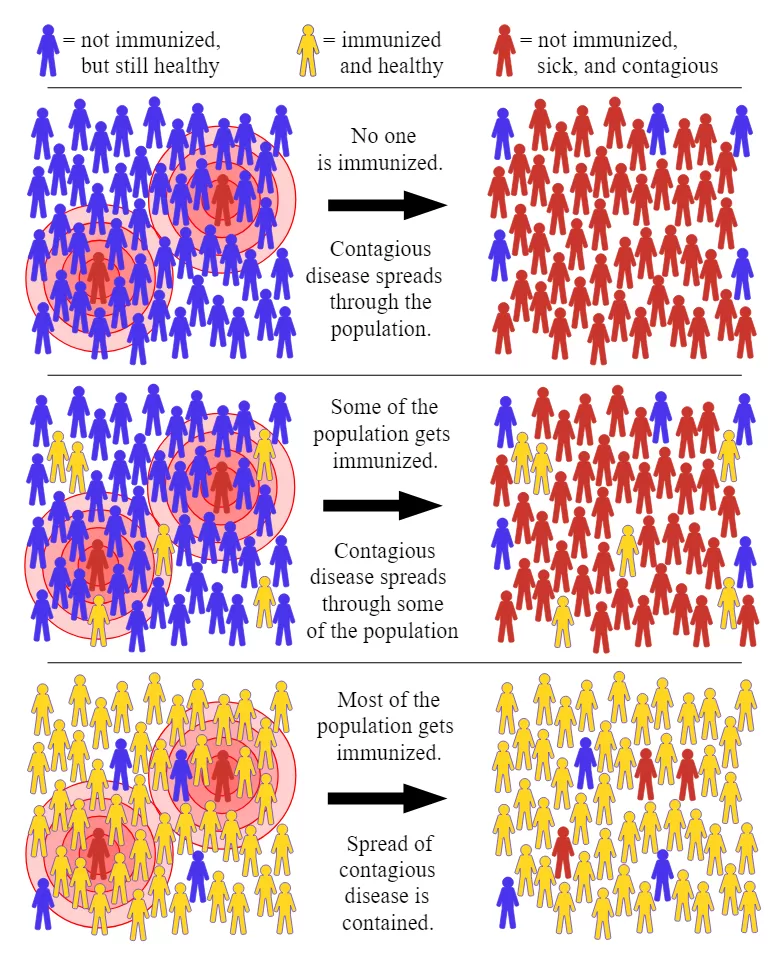
Herd immunity refers to a scenario where enough people in a population are immune to a particular disease, either through vaccination or prior infection, to prevent its spread. When a significant portion of the population is immune, either through natural immunity or vaccination, the disease has fewer opportunities to spread, effectively protecting the unvaccinated and vulnerable individuals.
In the context of infectious diseases, herd immunity is particularly important because it creates a form of indirect protection for people who cannot be vaccinated, such as individuals with weakened immune systems or those who are too young for certain vaccines. The level of immunity needed for herd immunity to take effect depends on how contagious the disease is.
For example, diseases like measles, which is highly contagious, require about 95% of the population to be immune to stop transmission. Other diseases, like COVID-19, have different thresholds, which are still being evaluated, especially as new variants emerge.
The Role of Vaccination in Achieving Herd Immunity
Vaccination is one of the most effective ways to build herd immunity. Vaccines stimulate the immune system to produce an immune response against specific pathogens without causing the disease itself. When a person is vaccinated, they gain immunity, which reduces the likelihood of transmitting the virus to others. Widespread vaccination across a population helps to decrease the overall spread of the virus, thereby protecting the community at large.
The success of COVID-19 vaccines, such as the Pfizer-BioNTech and Moderna shots, demonstrated how quickly mass vaccination efforts can lead to significant reductions in the spread of the virus. As vaccination rates increase, fewer people are susceptible to infection, and the virus has fewer hosts to spread to, thus lowering the overall rate of transmission.
How Many People Need to Be Vaccinated to Achieve Herd Immunity?
The percentage of the population that needs to be vaccinated for herd immunity to be achieved depends largely on the contagiousness of the disease. For example, diseases like measles, which has a basic reproduction number (R0) of around 12-18, require approximately 95% of the population to be immune in order to stop widespread transmission. This level is much higher than that of COVID-19, which has an R0 of 2-3, indicating that a lower percentage of immunity may be sufficient.
For COVID-19, the initial target was around 70-80% immunity to achieve herd immunity. However, new variants of the virus, such as Delta and Omicron, have caused this estimate to fluctuate. Experts suggest that to combat these variants, a higher level of vaccination, possibly 90% or more, combined with booster shots, will be necessary to reduce the spread effectively.
The CDC’s Current Recommendations emphasize not only completing the initial vaccination series but also receiving booster shots to maintain immunity and combat emerging variants. The rate of vaccination across the US varies widely by region, with some areas showing much higher rates than others, creating challenges for achieving nationwide herd immunity.
The Impact of Vaccine Hesitancy on Herd Immunity in the US
Despite the clear benefits of vaccination, the US faces significant challenges due to vaccine hesitancy. Distrust of the healthcare system, misinformation, and political polarization have all contributed to lower vaccination rates in certain communities. This has slowed progress toward achieving herd immunity, as pockets of unvaccinated individuals allow viruses to continue circulating.
The anti-vaccine movement has gained traction in the US, fueled by false claims about vaccine safety, and concerns over side effects, particularly with the rapid development of COVID-19 vaccines. According to the CDC, while the vaccine side effects are typically mild, such as sore arms or mild fever, misinformation about long-term effects and unfounded fears continue to dissuade many from getting vaccinated.
A report by the Kaiser Family Foundation (KFF) published in August 2021 found that political affiliation was one of the key factors influencing vaccine hesitancy. This divide presents a unique challenge for public health efforts, as vaccination is increasingly viewed through a political lens rather than a health and safety issue.
The Economic and Social Impact of Achieving Herd Immunity Through Vaccination
Achieving herd immunity not only benefits individual health but also brings significant economic and social advantages. Healthcare systems across the US have been severely strained during the COVID-19 pandemic, with hospitals facing overcrowding, particularly during surges in cases. Achieving herd immunity through widespread vaccination would help ensure that hospitals are not overwhelmed, and healthcare workers can focus on critical care rather than battling preventable diseases.
Economically, vaccination programs can help to restore stability. When people are vaccinated and protected from serious illness, workforce productivity improves, as fewer individuals fall ill and need to take time off. This leads to a more resilient economy, where businesses can operate normally without the risk of large-scale shutdowns due to COVID-19 outbreaks.
Additionally, public health costs can be reduced when disease outbreaks are minimized, as prevention is far more cost-effective than treatment. Vaccination programs, especially when they target communities most at risk, can save both lives and resources.
Timeline: The Road to Herd Immunity in the US
Early Vaccination Efforts:
- December 2020: The FDA grants emergency authorization for the first COVID-19 vaccines, including Pfizer-BioNTech and Moderna.
- January 2021: Mass vaccination begins in the US, initially prioritizing frontline healthcare workers and high-risk individuals.
Spring 2021:
- April 2021: Vaccine eligibility expands to all adults. Over 150 million Americans receive at least one dose of the vaccine by May 2021.
Summer 2021:
- As vaccination rates plateau, the Delta variant begins to cause concern. By July 2021, vaccine hesitancy has become a major barrier, and new efforts, including incentives and vaccine mandates, are introduced to boost vaccination rates.
Fall 2021:
- October 2021 sees the approval of booster shots for adults, aiming to enhance immunity, especially in the face of new variants.
2022 and Beyond:
- By 2023, despite significant progress, herd immunity remains elusive. Health experts emphasize the importance of boosters and continued public health campaigns to increase vaccination rates, especially in regions with low coverage.
Expert Opinions: What Experts Are Saying About Herd Immunity
Experts continue to debate the exact level of vaccination required to achieve herd immunity for COVID-19 in the US. Dr. Anthony Fauci, Director of the National Institute of Allergy and Infectious Diseases, has highlighted that while herd immunity is an ideal goal, it may not be a realistic one for COVID-19, particularly with the emergence of new variants. Instead, he advocates for maintaining high levels of vaccination and booster doses to mitigate the virus’s impact.
Dr. Walter Orenstein, a professor of vaccinology at Emory University, has stated, “We need to continue to focus on education and trust-building within communities to ensure that people understand the benefits of vaccination.”
In an interview with The New York Times in 2023, Dr. Orenstein emphasized that achieving herd immunity will not happen overnight and that sustained efforts are required to combat misinformation and increase public trust in vaccines.
Conclusion: Moving Forward
Reaching herd immunity in the US will require significant effort on the part of public health officials, healthcare workers, and the general population. Vaccination is the most effective tool in this fight, but vaccine hesitancy, misinformation, and political polarization remain significant obstacles. While the road to achieving herd immunity may be long, the economic, healthcare, and societal benefits of overcoming these challenges are immense. By continuing to push for higher vaccination rates, booster shots, and trust-building within communities, the US can make progress toward this crucial public health goal.
As experts agree, herd immunity is an ongoing process that will require continuous adaptation in response to emerging variants and new data. The key to success lies in collaboration, education, and a steadfast commitment to protecting the health of all Americans.
📚 Take Your Trading And Financial Skills to the Next Level!
If you enjoyed this post, dive deeper with our Profitable Trader Series—a step-by-step guide to mastering the stock market.
- Stock Market 101: Profits with Candlesticks
- Stock Market 201: Profits with Chart Patterns
- Stock Market 301: Advanced Trade Sheets
Start your journey now!
👉 Explore the Series Here
For Regular News and Updates Follow – Sentinel eGazette
FAQs:
Q1: What is herd immunity and why is it important for public health?
A1: Herd immunity occurs when a large portion of a community becomes immune to a disease, making its spread less likely. This protects vulnerable individuals who cannot be vaccinated, such as those with certain medical conditions or young children. Herd immunity is essential to stop epidemics and reduce the burden on healthcare systems.
Q2: How do vaccines contribute to achieving herd immunity?
A2: Vaccines create immunity in individuals without causing the disease. When a significant portion of the population is vaccinated, the disease has fewer opportunities to spread, helping to protect everyone, including those who cannot be vaccinated.
Q3: What is the ideal vaccination rate for herd immunity in the US?
A3: For COVID-19, experts initially estimated that 70-80% of the population needed to be vaccinated to achieve herd immunity. However, due to new variants, experts suggest that 90% or more might be needed for sufficient protection against transmission.
Q4: Why are some regions of the US struggling with vaccine hesitancy?
A4: Vaccine hesitancy in the US can be attributed to factors such as misinformation, political polarization, distrust in the healthcare system, and misconceptions about vaccine safety. These factors hinder efforts to achieve high vaccination rates and herd immunity.
Q5: How does vaccine hesitancy affect the goal of herd immunity?
A5: Vaccine hesitancy slows down vaccination efforts, preventing the population from reaching the necessary threshold for herd immunity. As a result, this prolongs the spread of diseases and poses a risk to unvaccinated or immunocompromised individuals.