Introduction: Female Reproductive Anatomy
The female reproductive system is a complex and essential part of the human body, responsible for processes like menstruation, reproduction, and hormonal regulation. By understanding its anatomy and functions, women and healthcare providers can take proactive steps in ensuring overall health and managing fertility. This in-depth guide will explore every aspect of the female reproductive system, from the external genitalia to the internal organs, hormonal functions, and key events that shape the reproductive lifespan.
Understanding the Basics of Female Reproductive Anatomy
The female reproductive system is made up of internal and external components, each playing an essential role in reproductive health. It is designed to perform complex functions, from menstruation to conception, and ultimately, childbirth. Understanding these functions is key to maintaining a healthy reproductive life.
The system includes:
- External Genitalia (Vulva)
- Internal Organs (Vagina, Uterus, Ovaries, Fallopian Tubes, etc.)
- Hormonal Regulation and its impacts on overall health.
These organs work synchronously, with hormones regulating the processes. Let’s break down these components in detail.
The External Genitalia: The First Line of Defense
The external genitalia, known as the vulva, serves as the body’s first defense against infections and physical injury. Comprised of several parts, the vulva protects the more sensitive internal structures and plays a key role in sexual arousal. Here’s a detailed look at the parts that make up the vulva:
- Mons Pubis: A fatty area located above the pubic bone. It’s covered with pubic hair during puberty and serves as a cushion during sexual activity.
- Labia Majora: The outer folds of skin that protect the internal structures. They also contain sweat and sebaceous glands, which help with lubrication.
- Labia Minora: These are the smaller inner folds of skin. The labia minora protect the urethra and vaginal opening.
- Clitoris: A highly sensitive organ designed for sexual pleasure. It has thousands of nerve endings and is considered the most sensitive part of the female anatomy.
- Vaginal Opening: The entry point to the vagina. The vaginal opening can expand during childbirth and sexual intercourse.
- Perineum: The region between the vaginal opening and the anus, which plays a role in childbirth, sometimes requiring an episiotomy during delivery.
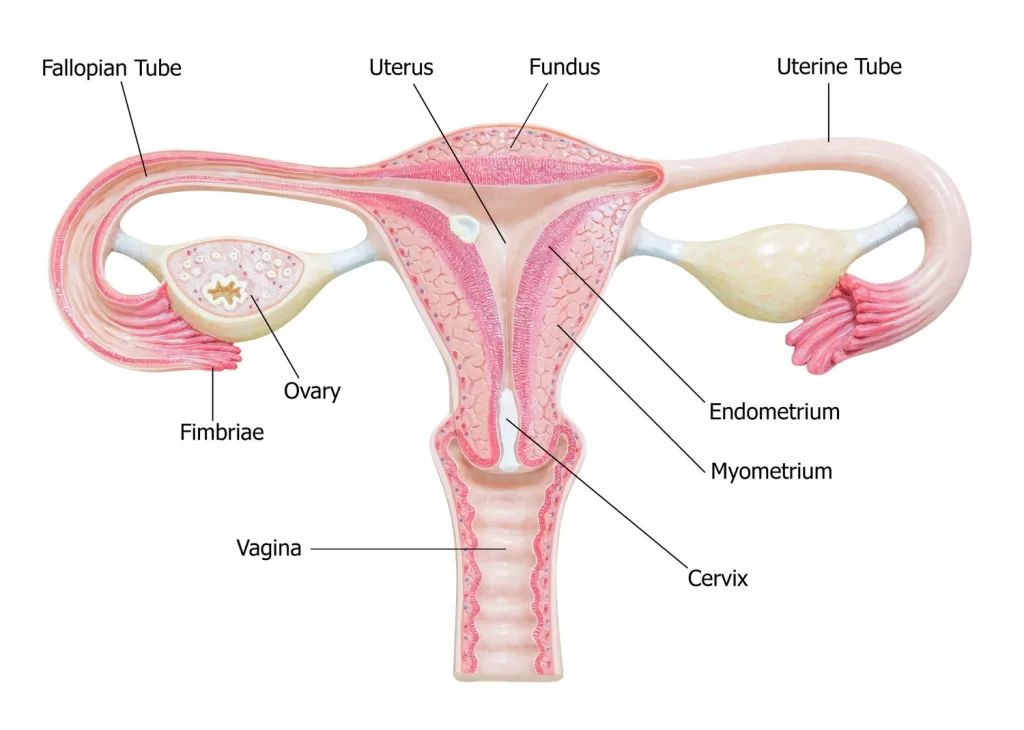
The Internal Organs of the Female Reproductive System
The internal organs are crucial to fertility, menstruation, and childbirth. These organs work together to ensure the proper functioning of the reproductive cycle:
- Vagina: A muscular tube that connects the uterus to the outside world. It serves as a pathway for menstrual blood to leave the body, as well as the passage for sexual intercourse and childbirth.
- Cervix: A narrow, cylindrical structure that connects the vagina to the uterus. The cervix secretes mucus that changes in consistency during different phases of the menstrual cycle, aiding in fertilization.
- Uterus: A hollow, muscular organ shaped like an upside-down pear. The uterus is where a fertilized egg implants and develops during pregnancy. The lining of the uterus (endometrium) thickens each month to support a potential pregnancy.
- Fallopian Tubes: These two tubes extend from the uterus to the ovaries and are the sites where fertilization usually occurs. They are lined with cilia that help transport the egg from the ovaries to the uterus.
- Ovaries: The female reproductive organs responsible for producing eggs (ova) and hormones. Each woman is born with a fixed number of eggs, and the ovaries secrete hormones such as estrogen and progesterone that regulate the menstrual cycle.
- Fimbriae: The finger-like projections at the end of the fallopian tubes. These catch the released egg and help guide it toward the fallopian tube for fertilization.
The Menstrual Cycle: A Hormonal Symphony
The menstrual cycle, lasting about 28 days on average, is a critical process regulated by hormones like estrogen and progesterone. These hormones control the development and release of eggs from the ovaries, the thickening of the uterine lining, and the shedding of that lining if no pregnancy occurs. The menstrual cycle involves four key phases:
- Menstrual Phase (Days 1-5): The shedding of the uterine lining, known as menstruation, occurs. This phase lasts about 3-5 days and is characterized by the flow of menstrual blood.
- Follicular Phase (Days 6-14): Estrogen levels rise, stimulating the growth of follicles in the ovaries. The endometrium thickens, preparing for a potential pregnancy.
- Ovulation (Day 14): A surge in luteinizing hormone (LH) triggers the release of a mature egg from the ovary. This is the period when the woman is most fertile.
- Luteal Phase (Days 15-28): The ruptured follicle becomes the corpus luteum and begins producing progesterone, which further thickens the uterine lining in preparation for pregnancy.
Functions of the Female Reproductive System
The functions of the female reproductive system are not limited to reproduction. These systems also maintain hormonal balance, regulate menstruation, and ensure a healthy sexual life. The four primary functions of the reproductive system are:
- Reproduction: The system’s primary function is to produce eggs and support pregnancy. The uterus provides the environment for the developing fetus, while the ovaries release eggs during the menstrual cycle.
- Hormonal Regulation: Hormones such as estrogen, progesterone, and LH play key roles in regulating the menstrual cycle, supporting pregnancy, and maintaining overall hormonal balance.
- Menstruation: If pregnancy does not occur, the endometrial lining is shed, leading to menstruation. This marks the reset of the reproductive system and the start of a new cycle.
- Sexual Health: The clitoris, vulva, and vagina all contribute to sexual pleasure. Healthy sexual function is an important aspect of overall reproductive well-being.
The Role of the Female Reproductive System in Pregnancy
Pregnancy begins when sperm fertilizes an egg. The fertilized egg travels to the uterus, where it implants in the thickened uterine lining. Pregnancy tests detect the presence of hCG, a hormone released by the placenta. The uterus undergoes many changes, with the growth of the placenta and the fetus. As the pregnancy progresses, hormones like estrogen and progesterone help maintain the pregnancy and prevent menstruation.
Expert Opinion: Dr. Laura Mitchell, a renowned obstetrician-gynecologist, explains, “The female body is equipped with extraordinary mechanisms that ensure both conception and the safe delivery of a child. From the release of the egg to the hormonal shifts during pregnancy, each step is critical for the successful development of a fetus.”
Timeline of Key Events in Female Reproductive Health
Age 8-13: Puberty begins. The first signs of puberty include breast development and the growth of pubic hair. Menstruation usually starts between ages 10-15.
Age 14-19: Menstrual cycles become more regular, although some irregularity may still occur in the early years of menstruation.
Age 20-35: Women experience peak fertility. Ovulation occurs regularly, and most women have few menstrual issues.
Age 35-40: Fertility begins to decline. Women may begin to notice changes in cycle length or volume of flow. The ovaries start releasing fewer eggs.
Age 45-55: Menopause marks the end of the menstrual cycle and fertility. Symptoms like hot flashes, mood swings, and vaginal dryness may occur as estrogen levels decrease.
Conclusion: The Importance of Female Reproductive Health
Understanding female reproductive anatomy is vital for overall health. From menstrual cycles to hormonal regulation, the reproductive system plays a pivotal role in women’s well-being. By keeping track of these processes, women can better manage their reproductive health, seek appropriate care when necessary, and enjoy a healthy, fulfilling life.
📚 Take Your Trading And Financial Skills to the Next Level!
If you enjoyed this post, dive deeper with our Profitable Trader Series—a step-by-step guide to mastering the stock market.
- Stock Market 101: Profits with Candlesticks
- Stock Market 201: Profits with Chart Patterns
- Stock Market 301: Advanced Trade Sheets
Start your journey now!
👉 Explore the Series Here
For Regular News and Updates Follow – Sentinel eGazette
FAQs:
Q1: What are the signs of a healthy menstrual cycle?
A healthy menstrual cycle typically lasts between 21 and 35 days, with a period of 3-7 days of menstrual bleeding. Regular cycles with minimal pain are signs of good reproductive health. If cycles become irregular or painful, it’s important to seek medical advice.
Q2: How do hormonal imbalances affect the female reproductive system?
Hormonal imbalances can lead to irregular menstrual cycles, difficulties in conceiving, or conditions like polycystic ovary syndrome (PCOS). Conditions like stress, diet, and health problems may cause fluctuations in hormones, impacting ovulation and fertility.
Q3: Can the female reproductive system be affected by age?
Yes, as women age, their fertility tends to decline. Around age 35, the quality of eggs declines, and the likelihood of miscarriage increases. Menopause, typically occurring between ages 45-55, marks the end of the reproductive years.
Q4: How can women maintain good reproductive health?
Maintaining a balanced diet, regular exercise, stress management, and routine gynecological check-ups are essential for reproductive health. Preventive care, such as getting vaccinated for HPV, also plays an important role in protecting against infections.
Q5: What are the primary functions of the ovaries in the female reproductive system?
The ovaries are responsible for producing eggs and secreting hormones like estrogen and progesterone. These hormones regulate the menstrual cycle and support pregnancy when an egg is fertilized.