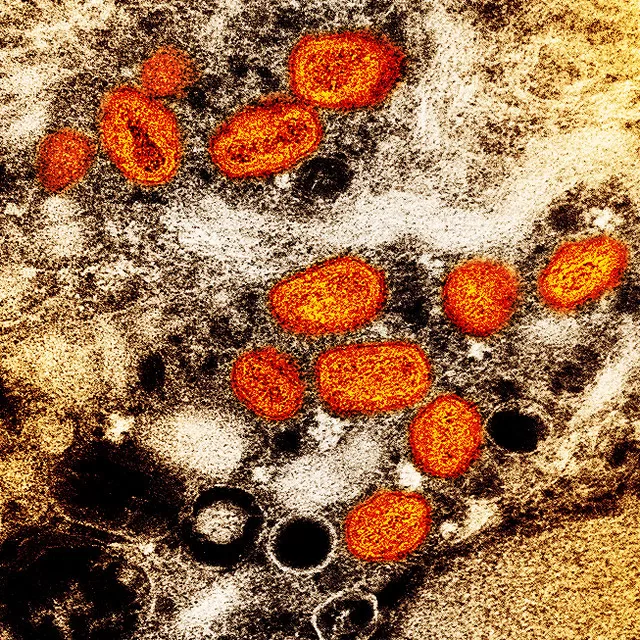
Introduction: Mpox Outbreak News
In a concerning development for public health, New South Wales (NSW) has reported its most significant outbreak of mpox to date, with health officials urging at-risk populations to prioritize vaccination. As of October 3, 2024, the state has recorded 433 confirmed mpox cases since June 1, 2024, marking a substantial rise in infections. Dr. Kerry Chant, the chief health officer of NSW, emphasized the seriousness of the situation, noting that 26 individuals have required hospitalization due to severe symptoms.
Rising Cases and Hospitalizations
The alarming spike in mpox cases has raised red flags for health authorities, with Dr. Chant describing the situation as “very concerning.” Most hospitalizations have occurred among individuals who have either received no doses of the vaccine or just one. In contrast, those who are fully vaccinated experience milder symptoms that typically last for a shorter duration.
In a detailed breakdown of the current cases, it has been reported that almost 40% of the infected individuals were fully vaccinated, while 14% had received just one dose. A striking 48% were completely unvaccinated, underscoring the urgent need for vaccination efforts.
Health experts highlight that, while the majority of cases are mild, the increase in hospitalizations calls for immediate action. Dr. Rohan Bopage, a specialist in sexual health at the Western Sydney Local Health District, noted, “While we are seeing mostly mild cases, the increasing number of severe cases is alarming. It’s essential for everyone, especially those in high-risk groups, to be vigilant and consider vaccination.”
Vaccination Drive for Vulnerable Populations
In response to the outbreak, NSW is offering two free doses of the mpox vaccine to high-risk groups, including men who have sex with men, sex workers, and their partners, regardless of their Medicare status. Individuals who have already received one dose are eligible for their second dose 28 days after the first.
Dr. Chant reiterated the message that while mpox can affect anyone, the virus is primarily transmitted through close skin-to-skin contact, particularly among men who have sex with men and sex workers. “We are urging them to complete their vaccinations, as two doses can provide vital protection against severe illness caused by the virus,” she stated.
Michael Woodhouse, the chief executive of ACON, a health organization serving LGBTQ+ communities in NSW, urged at-risk populations to take action. “Our communities have a long history of doing what it takes to protect ourselves and our partners. Now is one of those times. The vaccine is a key tool in our fight against mpox,” he explained.
National Context: Victoria’s Situation
The surge in mpox cases is not limited to NSW. In Victoria, 120 cases have been identified since April 2024, indicating a similar trend across the country. This year has seen a substantial increase in mpox cases in Australia, with the nation only recording 26 cases in 2023.
The rise in infections has prompted health authorities in both states to intensify their vaccination campaigns and outreach efforts. Dr. Chant emphasized the importance of education around the symptoms of mpox to help facilitate early detection and treatment. “People need to be aware that mpox is often accompanied by mild fever, headache, fatigue, swollen lymph nodes, mouth ulcers, and rectal pain,” she noted.
Understanding Mpox: Symptoms and Transmission
Mpox typically manifests with mild symptoms, often beginning with small pimple-like lesions on the skin. These can be accompanied by additional symptoms such as mild fever, headache, fatigue, swollen lymph nodes, mouth ulcers, and rectal pain. Health experts emphasize that the virus can also spread through sharing contaminated items such as bedding, towels, or clothing.
Dr. Rohan Bopage has cautioned individuals to be mindful of the conditions under which mpox spreads. “It spreads through close skin-to-skin contact, including sexual contact, and can also be transmitted through contaminated items,” he explained. He urged anyone who suspects they may have been exposed to mpox or who is experiencing symptoms to contact their GP or a sexual health service immediately.
Expert Opinions and Community Response
Dr. Chant has also noted that while NSW has not reported any cases of the new mpox virus strain, clade 1b, which has been observed in central and west Africa since January 2023, the risk remains present. Community health organizations are stepping up efforts to educate and inform at-risk populations about the importance of vaccination and awareness of symptoms.
Dr. Sophie Garcia, an infectious disease specialist, stated, “The community response has been critical. We are seeing people coming forward to get vaccinated, but we need to maintain that momentum to prevent further spread of the virus.”
Timeline of Events
- May 2022: First mpox case reported in NSW.
- June 1, 2024: NSW records 433 cases since this date.
- August 21, 2024: Victoria reports 120 cases since April.
- October 3, 2024: Current outbreak statistics confirmed by Dr. Kerry Chant.
Conclusion: A Call to Action
As NSW confronts its largest mpox outbreak, health officials are urging immediate action to mitigate the situation. With vaccinations being a key tool in combating the virus, it is crucial for at-risk individuals to participate in the vaccination drive. The recent surge in cases highlights the importance of public health initiatives in protecting vulnerable communities and ensuring the health and safety of all residents.
With these updates, it’s clear that public awareness, education, and vaccination efforts will play a pivotal role in controlling the mpox outbreak and safeguarding community health.
For Regular News and Updates Follow – Sentinel eGazette
FAQs
Q1: What are the main symptoms of mpox?
A1: Symptoms of mpox typically include mild fever, headache, fatigue, swollen lymph nodes, mouth ulcers, and pimple-like skin lesions.
Q2: How is mpox transmitted?
A2: Mpox is primarily spread through close skin-to-skin contact, including sexual contact, and can also be transmitted via contaminated items like towels and bedding.
Q3: Who is most at risk for mpox?
A3: Those at highest risk include men who have sex with men, sex workers, and their partners due to the close physical contact associated with these groups.
Q4: How effective is the mpox vaccine?
A4: The mpox vaccine has been shown to provide vital protection against severe illness, especially for those who receive both doses.
Q5: Where can I get vaccinated for mpox?
A5: Vaccination is available for high-risk groups at local health departments and clinics, regardless of Medicare status, to ensure accessibility.